Macular hole

The macular hole is a gap that occurs in the center of the retina, in the area called macula.

The retina is the light-sensitive tissue in the background of the eye.
In the early stages, the macula hole can cause blurred and distorted vision; straight lines may appear wavy or inclined and can be difficult to read.

Gradually a black spot appears in the center of vision or the patient simply fails to see in the center. It does not cause pain and the disease does not lead to complete loss of vision.
Surgery is usually required to repair the damage. The rate of anatomical success after surgery is about 90%.
Cause of macular hole: we do not know why macular holes develop; the vast majority of cases have no obvious cause; more often they affect people aged 60 to 80 years and are three times more common in women than in men. It is caused by a strong pull of the posterior vitreous in the macula area. Some cases may be related to retinal detachment or severe eye injury.
Diagnosis
In the appearance of blurred or distorted vision or black spot perception in the center of vision, immediate ophthalmological examination is required; without timely treatment the prognosis is usually very poor; there are cases such as post-traumatic holes where self-treatment may occur.
Treatment
Vitrectomy surgery is internationally, by far the most widespread and effective method of treatment. The operation is successful in closing the hole in about 9 out of 10 patients who have had a hole for less than 6 months. In a small number of patients, the hole does not close despite surgery and central vision may continue to deteriorate. However, a second operation may be successful in closing the hole.
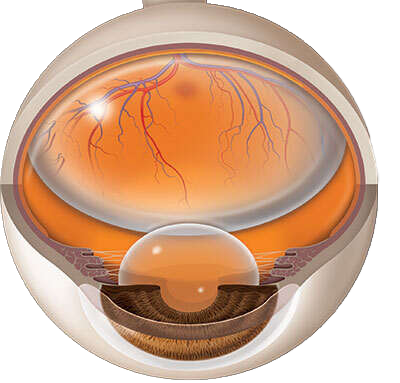
Operated eye with gas in the vitreous body
What is a vitrectomy?
The surgery of the hole of the macular is performed by use of a microscope. First the vitreous is removed and then a very thin layer (the inner limiting membrane) is carefully peeled from the surface of the retina around the hole in order to reduce the tangential forces that keep the hole open. Gas is then injected into the vitreous body. The gas bubble strongly restricts the vision but is absorbed within 15-20 days.
This operation usually lasts about half an hour under local anesthesia and does not require hospitalization.
Postoperatively
Temporarily poor vision. As long as the eye contains gas, the vision is impaired – such as when we are in the water.
Depth of field perception (three-dimensional vision) is significantly affected, so a lot of attention is required when walking.
At 7 to 10 days after the operation, central vision improves significantly.
Mild pain or discomfort. The eye is slightly irritated after surgery.
Contact the doctor immediately if:
- There’s intense pain.
- The vision worsens.
At the end of the operation usually the eye is covered for the same day only with a bandage. The next day the bandage is removed in the infirmary.
Medication: instillation of antibiotic and steroid collie.
Follow up: one day, one week and one month after surgery.
The first few weeks are required to avoid:
- eye rubbing
- Swimming
- intensive exercise
- eye makeup
In the first 3 days it is important to have a prone position for many hours of the day and for the first 5 days to completely avoid the supine position. There are indications that the prone position increases the success rate of the operation but may not be necessary in small holes. If a prone position is required, the head must be positioned so that the nose points towards the ground.
Travel: it is strictly forbidden to fly by aircraft and to go to an altitude of more than 300 meters from sea level.
Driving: driving is prohibited until vision is regained (approximately 8 days)
Work: if it is an office job it is allowed from the 4th post-operative day.
Possible complications: failure to close the hole, retinal detachment, infection, bleeding, cataract.
Cataract will almost certainly occur after months of if you haven’t already undergone cataract surgery.
Retinal detachment is performed in 1 to 2 out of 100 people undergoing macular hole surgery and requires surgical treatment.
Bleeding is very rare, as is the infection that occurs in about 1 in 5000 patients.
Success rate of the operation: the most important factor is the duration and size of the hole. Hole that exists for less than 6 months, has a 90% chance of healing; if the hole exists for a year or more, the success rate decreases to about 60%.
Probability of a macular hole in the other eye: 10%

